Author: Hannah
-

Everyday tales of trauma
A young woman who lost half her blood in a terrifying car crash, and lived. A man with a fractured skull from a simple fall on his stairs. A crack team of nurses, surgeons and specialists on call 24/7. Welcome to the daily drama of the region’s trauma HQ. It was late on a Thursday…
-
The numbers don’t lie
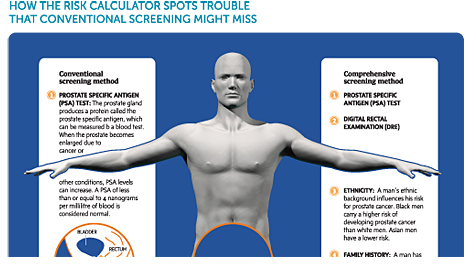
The day before Barry Shiffman was to fly from Toronto to Russia to begin serving on the Violin Jury of the International Tchaikovsky Competition, the 44-year-old learned he had prostate cancer. “I was floored by the diagnosis. I sat for in the lobby of Sunnybrook for two-and-a-half hours thinking, ‘What is happening?’” recalls Barry, who…
-

Despite Canadian government woes, neuroscience should win out
MONTREAL — When Canada’s Conservative government presented its 2011 budget in late March, the fiscal plan didn’t contain too many surprises for science funding. Like previous budgets, the proposal offered modest increases to the country’s national research agencies and replenished the coffers of Genome Canada, its genomics and proteomics outfit. But the budget also contained…
-

Canadian research shift makes waves
NRC Agency’s focus on industry-driven projects raises concerns that basic science will suffer. Published in Nature, 19 April 2011. Canada’s largest research entity has a new focus — and some disaffected scientists. On 1 April, the National Research Council (NRC), made up of more than 20 institutes and programmes with a total annual budget larger…
-
Think small
The Canadian forestry industry could hinge on the most abundant nanomaterial on earth. A pale grey slurry roils about in a waist-high blue plastic drum at the centre of a garage-like space at the National Research Council’s Biotechnology Research Institute in Montreal. It looks a little like slush, but when it is dried it more…